Friday, July 31, 2015
Thursday, July 30, 2015
How immigrants help health reform succeed
Medicare turns 50 today, which has provided an opportunity for all manner of retrospectives and speculation about what the future holds. The Partnership for a New American Economy is publicizing one of my favorite arguments: that immigrants are a key reason that Medicare is still solvent.
Their 2014 study (Staying Covered: How Immigrants Have Prolonged the Solvency of One of Medicare’s Key Trust Funds and Subsidized Care for U.S. Seniors) concludes:
- Immigrants are subsidizing Medicare’s core trust fund
- Immigrants played a critical role subsidizing Medicare’s Hospital Insurance Trust Fund during the recent recession
- Medicare’s Hospital Insurance Trust Fund would be nearing insolvency if not for the contributions of immigrants in recent years
Bottom line: immigrants contributed $182 billion more to the Hospital Insurance Trust Fund between 1996 and 2011 than they received in benefits. Meanwhile, US-born citizens sucked out $69 billion more than they paid in.
But the argument for open integration goes far beyond the Medicare story. As I wrote back in 2011 (We need a liberal immigration policy to support health care reform)
- Immigrants innovate and create economic growth. This growth is how the country gets wealthier and better able to support health care expenses without raising tax rates
- Immigrants can use their intellectual capital and training –whether acquired abroad or here– to fill healthcare jobs such as primary care physician, pharmacist, nurse that would otherwise go unfilled
We have very stupidly made the US less welcoming to immigrants at the same time that talented people have more opportunities in their birth countries and while other countries have made it easier for educated immigrants to thrive. I partly blame the current state of affairs on the post-9/11 mentality. We’ll pay for it in the long run in healthcare and in the economy at large.
Image courtesy of Stuart Miles at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/30/how-immigrants-help-health-reform-succeed/
via A Health Business Blog
Wednesday, July 29, 2015
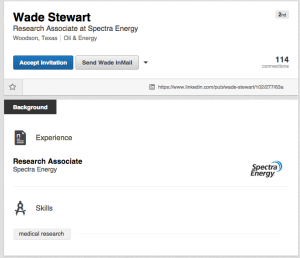
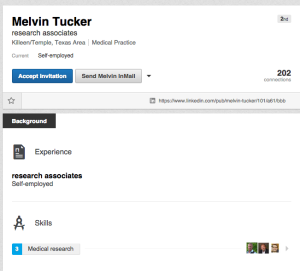
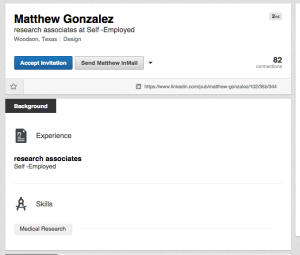
Why am I getting so many spam invites on LinkedIn?
Over the last few days I’ve received several LinkedIn requests that don’t look real. Typically they are from “people” with the title of Research Associate or something similar. When I view the profile there is almost nothing there. However, they usually have at least one other connection with someone in my network. Here are a few examples — I’ve left off the connections we have in common so as not to embarrass anyone who’s blindly accepting LinkedIn invites.
My best guess is this is some sort of spam or phishing attempt. I’ve been reporting these profiles to LinkedIn but so far no acknowledgment from them and no way to connect with them by phone.
Anyone else seeing this? Leave a comment or tweet to @HealthBizBlog.
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/29/why-am-i-getting-so-many-spam-invites-on-linkedin/
via A Health Business Blog
Tuesday, July 28, 2015
Monday, July 27, 2015
Four reasons Praluent is not Sovaldi
From the New York Times (New Drug Sharply Lowers Cholesterol, But it’s Costly)
Praluent, which analysts project will become a huge seller, is expected to become the next flashpoint in the growing controversy of escalating pharmaceutical prices, and health plans are expected to put in place strict measures to control which patients can use the drug and prevent it from becoming a budget buster.
This story and similar ones say Praluent may be like Sovaldi, an expensive Hepatitis C drug that has driven up healthcare costs over the past year or so. According to this narrative, health plans and pharmacy benefits managers are gearing up to do battle with the manufacturer and have learned their lesson from the Sovaldi experience. Maybe the payers will do a better job of managing Praluent expenses –I assume they can devise something better than whining about the expense to the general public while simultaneously rallying against price controls. But when the Praluent crisis is “averted” don’t let the payers pat themselves on the back too much.
I see four main reasons why Praluent will not be as much of a “budget buster” as Sovaldi:
- Praluent doesn’t cure anything
- There are good alternatives for most patients
- Praluent is an injection
- Praluent will have competition from the start
1. Praluent doesn’t cure anything
Sovaldi cures Hepatitis-C in something like 90 percent of patients. You can quibble with the numbers if you like, but the fact is this is a cure for many people who have waited for one –in many cases for decades. Take it for three months and you’re done with the drug and the illness.
What does Praluent do? It lowers cholesterol dramatically. Does it prevent heart attacks or strokes? No one knows, and we won’t have evidence about that for a couple years at least. In any case I’m sure it won’t cure heart attacks or strokes and I doubt it will reduce their likelihood by anything approaching 90 percent. And patients will have to keep using the drug indefinitely.
2. There are good alternatives for most patients
Statins work well and are available as inexpensive generics. Starting on a statin or increasing statin dosage is an option for most patients, including those who have already had a stroke or heart attack. A smaller group has a genetic condition that can’t be addressed by statins. Praluent sounds like a good choice for them.
3. Praluent is an injection
Sovaldi comes in a pill. It’s easy to swallow. Same with statins.
Praluent is an injection. Ouch. Sure it only has to be done twice a month and you can do it yourself, but who really likes a needle? I expect patients to want to try statins first.
4. Praluent will have competition from the start
Sovaldi was on the market for about a year before an (arguably inferior) competitive offering was introduced. That gave Gilead a big first-mover advantage, especially important for a drug people had been awaiting for a long time and then only needed to take for three months.
It appears that Repatha, a similar drug to Praluent, will come to market about the same time, with others to follow. Competitive pressures should keep prices in check.
5. The name evokes something nasty
I know I promised only four reasons, but I have fifth. The name reminds me too much of Soylent, the disgusting meal replacement product.
Image courtesy of digitalart at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/27/four-reasons-praluent-is-not-sovaldi/
via A Health Business Blog
Saturday, July 25, 2015
Friday, July 24, 2015
par8o and IRCDA team to automate clinical assessment with SCAMPS
par80 and the Institute for Relevant Clinical Data Analytics (IRCDA) have teamed up to enable sophisticated clinical decision support at the point of care using SCAMPS. I asked Dr. Adam Sharp, par80’s cofounder, president and chief medical officer to explain.
- What are SCAMPs? How do they differ from evidence-based protocols?
- SCAMPs are Standardized Clinical Assessment and Management Plans. SCAMPs outline a data-backed, consensus-based, care pathway for a diverse patient population with a particular diagnosis or condition. Data is collected on the treatment and outcomes of that population, analyzed, and then used to improve the care pathway
- While evidence based protocols can answer highly specific medical questions, the traditional methods are inadequate to address the interdependent questions related to defining effective care
- SCAMPs aim to bridge the gap with a method that is integrally linked to continuous improvement
- Additionally, SCAMPs aim to reduce the cost of delivering care to patients while improving quality by focusing on standardization of care and reduction of unnecessary utilization
- What are some examples of SCAMPs? What value do they provide?
- There are a wide variety of SCAMPs, ranging from the inpatient to outpatient to ER settings. Some examples of SCAMPs are the Congestive Heart Failure SCAMP (inpatient) Distal Radius Fracture (outpatient), and Acute Kidney Injury (ICU)
- They reduce variability in care. The algorithm drives consistency among participating providers. In addition to providing a layer of liability protection, organizations want to drive towards best practice guidelines. SCAMPs do so from the grassroots level
- SCAMPs gain support from providers because in spite of a foundational algorithm driving decisions, providers are free to diverge from the SCAMP recommendation, so long as they provide a reason. This empowers providers to use their own intelligence alongside the best practice guidelines laid out by the SCAMP
- Finally, a SCAMP is never perfect. After using it in the field for a given amount of time, the data is collected and analyzed by IRCDA’s analytics team. The output is then used to reevaluate the SCAMP and to change the algorithm to account for the decisions doctors made. These iterations ensure care pathways are constantly improving based on the latest empiric evidence
- And what is IRCDA? How does it relate to SCAMPs?
- IRCDA is the Institute for Relevant Clinical Data Analysis. In 2006, clinicians in the Cardiology Department at Boston Children’s Hospital began to toy with a new methodology. This methodology would ultimately create SCAMPs
- As success grew and institutions around the world became interested, IRCDA was created in 2010 to spread and promote SCAMPs to interested institutions
- You’re a founder of par8o, which you describe as a healthcare operating system. You’re partnering with IRCDA to implement SCAMPs. How does all of this fit together? If par8o is the operating system, what does that make IRCDA, SCAMPs, and hospitals?
- IRCDA, SCAMPs, and hospitals in many ways represent a microcosm of the healthcare system as a whole. A major benefit of working with IRCDA is that it touches so many major components of the healthcare industry
- It ranges across healthcare settings (inpatient, outpatient, ER) in addition to focusing on the most important players in the industry – the providers
- As healthcare’s operating system, par8o wants to layer itself onto as many aspects of care as possible. Doing so will allow us to bring efficiency to all parts of the industry
- Finally, pathways in healthcare are manifold. From taking a patient through the right care pathway, to following a pathway created by an insurance company for specialty pharma, to finding eligible patients for clinical trials, the foundation par8o builds with care pathways will have many implications for driving efficiencies in other aspects of healthcare
- How are EMRs involved in this initiative?
- par8o integrates with all EMRs via the Direct protocol developed by HHS Office of the National Coordinator (ONC). SCAMPs can be initiated out of an EMR using a direct message – the direct message will trigger a draft SCAMP to be created in par8o and will notify the provider that they must complete the SCAMP
- Therefore, so long as the EMR supports Direct messaging, par8o can use that functionality to integrate
- What impact will this partnership have for patients?
- Patients will benefit because par8o’s technology will address two key pain points currently in the SCAMP process. The first is unwieldy data entry – par8o will enable providers to complete SCAMPs from their mobile phone. Using decision support, the forms will seem less onerous
- Additionally, by leveraging form versioning technology, par8o will enable faster iterations on SCAMPs. Faster iterations means the data gathered during SCAMP collection can be leveraged sooner, resulting in enhanced care for affected patient populations
- This is clearly a first step. How do you see development rolling out over the next few years?
- Over the next few years, par8o has a big vision. To start, our aim is to successfully launch a pilot program at a single institution. We hope to ease data entry issues and therefore increase adoption. Additionally, we hope to see faster iterations between SCAMP versions
- In the future, in addition to expanding to more member institutions, we would like to see a social element brought to SCAMPs where providers are able to participate in chat forums and share the latest literature concerning that area of care
- par8o also plans to build a SCAMPs “Editor”, which would enable the IRCDA team to build and version their own SCAMPs, greatly increasing the iteration process
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/24/par8o-and-ircda-team-to-automate-clinical-assessment-with-scamps/
via A Health Business Blog
Thursday, July 23, 2015
Wednesday, July 22, 2015
Fast progress on transgender benefits
Bruce Jenner’s transition to Caitlyn Jenner has brought transgender issues quickly to the fore. What I had not realized is that major employers and the federal government are well on their way toward providing coverage for transition-related health care. I’m not in a position to comment on the adequacy of the coverage, but just want to make the point that it’s advanced faster than I thought.
According to Business Insurance (Transgender benefits gain attention of employers), the Office of Personnel Management recently required Federal Employee Benefit Plan providers to cover transition-related care, citing an emerging consensus that such treatment is medically necessary.
About half of large employers offer transgender-related surgical coverage compared with 5 percent in 2007, according to a National Business Group on Health survey.
Transgender-related benefits are varied, and include “mental health counseling, hormone replacement therapy and gender reassignment surgery. Some employers… include coverage for facial feminization or reducing the Adam’s apple…” Not every employer offers all categories of benefits.
Private employers aren’t required by law to offer such benefits, but they have various motivations. They include:
- An increasing belief that such coverage is medically necessary, and therefore in keeping with the overall philosophy of health insurance
- A desire to increase competitive positioning in recruiting –including for employees that do not themselves expect to use such coverage but are looking for employers that are progressive
- A realization that the overall costs are likely to be small, typically less than 0.5% of total health care costs
- A defensive view that not offering such benefits could lead to discrimination claims
I don’t typically think about insurance benefits being in the social and cultural vanguard, but at least based on this example that may not be a fair assessment.
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/22/fast-progress-on-transgender-benefits/
via A Health Business Blog
Tuesday, July 21, 2015
Monday, July 20, 2015
Follow-on biologics: Another ho-hum assessment
Proponents of follow-on biologics are invariably surprised that their hopes for product introductions and price competition outpace reality. Instead of stepping back and asking whether the whole concept of biosimilars makes any sense from a cost reduction standpoint they persist in recommending tweaks to the existing regime and asking for patience as we await results.
The New England Journal of Medicine published a Perspective on the topic last month (Progress and Hurdles for Follow-on Biologics), which followed the usual script. Rather than blog about it I wrote a letter to the editor. I didn’t expect to see it published –after all NEJM receives lots of letters and I don’t have the right academic credentials. Sure enough it was rejected, so here it is:
Sarpatwari et al. (June 19 issue) mistakenly expect the market for follow-on biologic drugs to evolve in a similar manner to the market for generic versions of small molecules. As a result they are surprised that prices of follow-on biologics are stubbornly high and competition low. But follow-on biologics are more like me-too versions of small molecule products, where similar drugs are introduced in the same class. Remember, Lipitor was a me-too product, the fifth statin on the market. Lipitor didn’t compete on price, however. Instead Pfizer used superior marketing to differentiate. I expect similar behavior in biologics.
The authors’ misunderstanding leads them to faulty recommendations designed to encourage development of more follow-on products. If the goal is to reduce costs without depressing innovation, then a wiser approach would be to regulate the price of the original biologic after it has been on the market for a decade or so. That would enable innovators to earn healthy financial returns, eliminate the expense and risk to patients of clinical trials of follow-on products, and reduce demands on FDA inspectors.
David E. Williams, MBA
Health Business Group
Boston, MA
Image courtesy of stockimages at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/20/follow-on-biologics-another-ho-hum-assessment/
via A Health Business Blog
Friday, July 17, 2015
An inspiring product development tale
The times they are a changing, and in some ways for the better. Nike is releasing a new sneaker designed for people with disabilities who have trouble putting regular shoes on by themselves. The idea for the shoe came from a teen with cerebral palsy who wrote a letter to Nike that ended up with the CEO. A related request came from a Nike employee who had suffered a stroke.
The company then spent three years to design a sneaker with what USA Today calls “an elongated wraparound zipper system to allow a wearer to open close the show with one hand.” They collaborated with the teen to perfect the design.
This isn’t some clunky looking, medicalized shoe. Instead, the Zoom Soldier 8 Flyease is a variation on a Lebron James basketball shoe. It’s cool and stylish.
Advocates for the disabled are pleased, because Nike can make a significant impact on quality of life with this product, and because it represents a new phase of acceptance for people who are a little different. I won’t be surprised if the shoe is a big hit –there are lots of people who have physical challenges of various types who might really like it.
If Nike can make money on the concept, that’s good news for everyone because it will demonstrate that this is a profitable opportunity, which will encourage others to compete.
The situation reminds me somewhat of the highway safety movement a generation ago. Although the problem of avoidable automobile deaths was there if you looked for it, the auto industry –with the exception of Volvo– wanted nothing to do with it. But once the public started to express an interest in safety, the world changed, and car companies started to compete on safety as well as styling and power.
Image courtesy of David Castillo Dominici at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/17/an-inspiring-product-development-tale/
via A Health Business Blog
Thursday, July 16, 2015
Health Wonk Review is up at InsureBlog
InsureBlogger Hank Stern takes over as curator and bartender for the latest edition of the Health Wonk Review blog carnival. You’ll find a great collection of health policy posts there.
Image courtesy of Stuart Miles at FreeDigitalPhotos.net
from Health Business Blog http://healthbusinessblog.com/2015/07/16/health-wonk-review-is-up-at-insureblog-15/
via A Health Business Blog
Wednesday, July 15, 2015
How narrow is a narrow network?
Health Insurance Exchanges are one of the most interesting and potentially impactful features of the Affordable Care Act. The exchanges allow eligible individuals to compare health plans on an apples-to-apples basis and choose the one that’s most appropriate for their individual circumstances.
Health plans are interested in participating in these exchanges because they offer one of the few sources of member growth. Federal subsidies make exchange plans affordable for middle income buyers who make too much to qualify for Medicaid.
Not surprisingly, exchange customers are price conscious shoppers. That means plans have to work hard to offer low enough premiums to be competitive. The Affordable Care Act outlaws some of the ways health plans used to stay competitive, such as charging different prices based on health status, refusing to cover certain patients, making exclusions for pre-existing conditions, and offering skinny benefits packages.
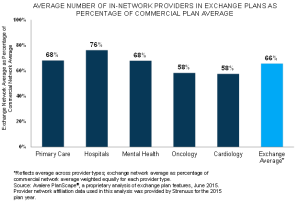
One of the few things plans can do is to offer different networks of physicians, hospitals and other providers. Exchange plans have embraced the concept of “narrow networks,” which offer a smaller than usual collection of providers as a way to hold down costs. I have heard and seen a lot of anecdotes about what this means in practice, but now there is some real data.
Avalere has conducted an analysis of health plans in the top five exchange states to compare the size of exchange plan networks with the size of commercial networks in the same geographies. Sure enough, the plans included an average of 34 percent fewer providers on average, and 42 percent fewer oncologists and cardiologists.
Although anyone’s initial reaction is that a bigger network is better, that is not automatically the case. If the narrower networks exclude the wasteful, low quality providers the result could be increased quality and cost effectiveness. If network inclusion is based just on unit costs, then who knows the outcome on quality. And if fewer providers means it’s harder to get an appointment, that could be problematic. Patients might even end up spending out-of-pocket for out-of-network coverage.
I asked Avalere vice president Elizabeth Carpenter to answer a few questions that immediately came to mind: You report the average, but how much variability is there? How have network sizes changed since last year? How often do exchange members go out-of-network?
Elizabeth answered the first question as follows, “Overall, we did see noticeable variation among the five states we examined. However, interestingly, it was not consistent across provider type. For example, exchange plans in one state may cover a higher percentage of primary care physicians than another state’s exchange plans but may cover a lower percentage of hospitals.”
As I expected, Avalere hasn’t yet done the work to answer the other questions. Clearly there are lots of interesting studies to be done on the impact of exchange plans on costs, quality, and the overall insurance market. I eagerly await them.
Image courtesy of marcolm at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/15/how-narrow-is-a-narrow-network/
via A Health Business Blog
Tuesday, July 14, 2015
This #stingray with a carbon fiber body kit is sick!

This #stingray with a carbon fiber body kit is sick!
from Discount Store Returns Blogger blog http://discountstorereturns.blogspot.com/2015/07/this-stingray-with-carbon-fiber-body.html
via Discount Store Returns Blogger Blog
Sunday, July 12, 2015
Friday, July 10, 2015
Checking the symptom checkers
Online “symptom checkers have deficits in both diagnosis and triage, and their triage advice is generally risk averse,” according to a new study in BMJ by Harvard researchers. Some of the press coverage of the study has been pretty critical of the symptom checkers, but the study itself is quite balanced.
Symptom checkers are a lot better than “Google Diagnosing” (typing a list of symptoms into Google and seeing what comes up). They’re very similar to nurse triage lines used by health plans, which is no great surprise considering that many of the triage lines use the same logic that drives the symptom checkers. They’re inferior to a primary care physician, but of course physicians aren’t infallible either.
People use symptom checkers to self-diagnose and to figure out if they need to go the emergency department, doctor’s office or can treat at home. Not surprisingly, the symptom checkers err on the side of suggesting patients seek care. No producer of these tools wants to get sued for recommending self-care to someone who should have called an ambulance. But in this regard symptom checkers are similar to nurse triage lines and also –at least in my experience– to physicians who are covering call. Too often they suggest a trip to the ED.
There’s an opportunity to reframe the next generation of symptom checkers as tools for navigating the medical system. That means not just suggesting a diagnosis and level of care, but pointing to an appropriate specialty, facility, or individual clinician to follow up with. This could be especially useful for patients in areas with fewer specialists and sub-specialists, and those with rare or hard to diagnose conditions. Primary care physicians could use such a tool as well to help direct referrals.
Image courtesy of David Castillo Dominici at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/10/checking-the-symptom-checkers/
via A Health Business Blog
Thursday, July 9, 2015
The specialty drug pricing conundrum: Caps may raise costs, not lower them
It used to require hundreds of thousands of patients taking a drug to make it blockbuster. But over the last decade drug companies have figured out that they can get to $1 billion in product sales with much smaller populations. The key: sky-high prices.
The math is simple. A drug that goes for $1000 per year needs 1 million patients to get to the billion dollar mark, but if the price is $100,000 it takes just 10,000 patients. At $200,000 it’s 5000. Anyway, you get the idea.
You don’t see these dynamics in other fields, but healthcare is different. The two big drivers: third-party payment that shelters patients from the real costs of treatments and an aversion to talking about anything that could be construed as “rationing.”
In fact, as Kaiser Health News reports (States Limiting Patient Costs For High-Priced Drugs) public policy is moving even further away from using cost-sharing to constrain demand by limiting out-of-pocket payment amounts to as low as $100 per month. These policies will backfire as cost containment mechanisms because they will just end up boosting premiums.
Some other states are considering bills to require manufacturers to report their costs for high-priced drugs. That strikes me as pretty useless as well. If it’s a first step toward capping prices, that may discourage companies from moving forward with risky development programs for orphan diseases.
So what can be done, if anything? Well, a few things:
- Use step therapy and similar programs to try less expensive treatments before defaulting toward the priciest. These programs are used today, but too often patients jump right to the high-priced specialty drug without seeing if something else would work
- Shift the site of service for infused drugs away from hospital outpatient settings toward the home or physician’s office, which is much less costly
- Encourage comparative effectiveness research and the adoption of quantitative measures such as Quality Adjusted Life Years (QALYs) to compare the efficacy of different treatments
- Demand real-world, patient outcomes data from marketed products
- Once a specialty (biologic) product has been on the market for several years and its patents have expired, regulate its price. This is a safer, more cost effective approach than encouraging so-called biosimilars
Image courtesy of Salvatore Vuono at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/09/the-specialty-drug-pricing-conundrum-caps-may-raise-costs-not-lower-them/
via A Health Business Blog
Wednesday, July 8, 2015
Tuesday, July 7, 2015
Monday, July 6, 2015
Partners HealthCare goes global: Is it a good idea?
In shift, Partners HealthCare seeking growth globally in today’s Boston Globe describes how Partners is turning its focus from dominating the Massachusetts healthcare delivery system to looking for revenue growth overseas.
This wasn’t hard to predict, and it makes a good deal of sense. Last year the Globe asked me to speculate on whether Partners’ hiring of a new CEO would change the company’s strategic course. I said it was surprising that Partners had continued its relentless expansion in Massachusetts. While it made sense to affiliate with community hospitals and physician practices to generate complex referrals for “tertiary” care, it was puzzling why Partners wanted to be in the business of offering the most cost-effective colonoscopies and other routine services throughout the state, generating friction with the state government, health plans, employers and consumers as a byproduct.
I suggested that Partners might choose to return to its roots as a world-renowned academic medical center with its Massachusetts General and Brigham and Women’s hospitals. Interestingly, from today’s article it appears that MGH and the Brigham –not Partners itself– are the entities that are driving forward. MGH plans to manage a hospital in China near Macau while the Brigham has recruited a chief business development officer from Johns Hopkins to set up business in the usual hotspots for high-dollar international medical ventures, i.e., China and the Persian Gulf, with a nod toward emerging South American economies.
Using the MGH and Brigham brands is wise, and helps remind us of just what Partners is. Remember, Partners was established to prevent health plans and the state from playing MGH and the Brigham off of one another in contract negotiations. The two hospitals continue to exist –it is not a merger in the traditional sense.
But these entities will have to be careful when they go abroad prospecting for gold. A few things to watch out for:
- Politics: Picking one foreign partner in a region can mean foregoing the opportunity to work with that entity’s rivals. And if an emir is ousted his successor may shoot down the pet projects of the previous emir and his family. (It has happened!)
- Brand risk: When I traveled to Asia a decade ago to research medical tourism, the Harvard name and crest were splashed up all over the place by operators who had little or nothing to do with Harvard. That had something to do with an earlier venture by Partners hospitals to use the Harvard name to drum up business overseas. It worked a little too well.
- Overconfidence: Sure we have great hospitals here in Boston. But not everyone running a hospital overseas is an idiot; many understand their own health system and patient populations pretty well. When I visited Singapore hospitals I was struck by the openness of executives in speaking with me, and impressed with their approach to cost-effective, high quality care. The one exception was when I visited a Hopkins outpost there, where the staff were highly bureaucratic and unapproachable. MGH and the Brigham will need to make sure what they take on is aligned with their true areas of differentiation and not just their self-perceptions.
- Ethical risk: Let’s be honest. American values differ from those of the Persian Gulf and China. As just one example, anyone in Boston can show up at the emergency department of MGH or the Brigham and be treated, regardless of nationality, race, religion or ability to pay. Will that be the case in hospitals MGH and the Brigham work with overseas? If not, is that ok? What else needs to be considered?
I wish the MGH and Brigham well in their overseas forays, and do think it’s a more fruitful approach than further expansion in Massachusetts. The Globe should have plenty more to write about as the strategies unfold.
Image courtesy of pakorn at FreeDigitalPhotos.net
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/06/partners-healthcare-goes-global-is-it-a-good-idea/
via A Health Business Blog
Saturday, July 4, 2015
Friday, July 3, 2015
Thursday, July 2, 2015
Wednesday, July 1, 2015
Partners closes Lynn’s hospital. I’m quoted
Partners is following through on a plan to consolidate its North Shore operations into Salem Medical Center, a move that will result in the closure of Union Hospital in Lynn, 6 miles away. I’m quoted in the print edition of the Boston Globe (Partners to close Union Hospital in Lynn) although as of 7 am the online version has not yet been updated.
Here’s what I had to say:
David E. Williams, president of Health Business Group in Boston, said Union’s closing is hardly surprising, since many community hospitals –particularly those that treat high numbers of low-income patients and rely on government reimbursements– are struggling financially.
He said Partners, the state’s largest health system, is closing the hospital more gently than other health care companies without as much money; keeping an emergency room open for three years is a big concession to community concerns.
“I do largely buy their logic,” Williams said about Partners. “On the one hand, nobody likes it when their local hospital closes. On the other hand, considering how high health care costs are, it can’t say the way it is.”
—
By healthcare business consultant David E. Williams, president of Health Business Group.
from Health Business Blog http://healthbusinessblog.com/2015/07/01/partners-closes-lynns-hospital-im-quoted/
via A Health Business Blog